Contrary to popular belief, the greatest heart danger from smoking isn’t a long-term risk; it’s the immediate, violent reaction in your blood that happens within minutes of every cigarette.
- Just 4-6 cigarettes a day still nearly doubles your mortality risk compared to never smoking.
- Quitting provides a greater cardiovascular risk reduction (up to 44%) than starting a statin medication (25-30%).
Recommendation: Focus on complete cessation, as even “light” smoking maintains a state of high alert in your cardiovascular system, preventing true recovery.
If you’re over 50 and a smoker, you likely live with a low-level hum of anxiety about your heart. A strange flutter in your chest, feeling winded after climbing stairs, or a family history of heart disease can turn that hum into a roar. You’ve heard the generic advice to “quit” countless times, but it often feels abstract, and a nagging voice might whisper that the damage is already done. Many patients I see believe that cutting down is a reasonable compromise, a way to mitigate risk without the difficult process of quitting entirely.
But what if the fundamental way you think about smoking and heart risk is flawed? The danger isn’t some far-off statistical probability that builds over decades. It’s a physical, mechanical event that happens inside your arteries with every single cigarette. The true key to protecting your heart isn’t just about reducing a long-term risk number; it’s about stopping an immediate, ongoing assault on your cardiovascular system. Your body has a remarkable capacity to heal, but it cannot begin this process in earnest while still under daily attack.
This article moves beyond vague warnings. As a cardiologist specializing in risk reduction, I will provide you with a clear, science-backed timeline of what happens inside your body from the very moment you extinguish your last cigarette. We will explore the immediate changes in your blood, the battle between different types of arterial plaque, and why quitting is a more powerful intervention for your heart than even some prescription medications. Understanding this timeline is the first step toward taking decisive, empowered action for your future.
To fully grasp the journey from risk to recovery, this article is structured to walk you through the critical biological processes and milestones. The following summary outlines the key areas we will explore, giving you a clear roadmap to understanding how your body can—and will—begin to heal.
Summary: Your Heart’s Recovery Timeline After Quitting
- How Smoking Thickens Your Blood Instantly and Causes Clots?
- Statins or Quitting: Which Reduces Cardiovascular Risk More?
- Tracking Your BP: How Much Does It Drop 2 Weeks After Quitting?
- Why “Cutting Down” to 5 Cigarettes Doesn’t Protect Your Heart?
- Vitamins and Supplements That Support Artery Health During Recovery
- Soft Plaque vs Hard Plaque: The Ticking Time Bomb in Smokers
- Why You Feel Tired All Day Despite Sleeping 8 Hours?
- Silent Ischemia: Why Your Heart Suffers Even Without Chest Pain?
How Smoking Thickens Your Blood Instantly and Causes Clots?
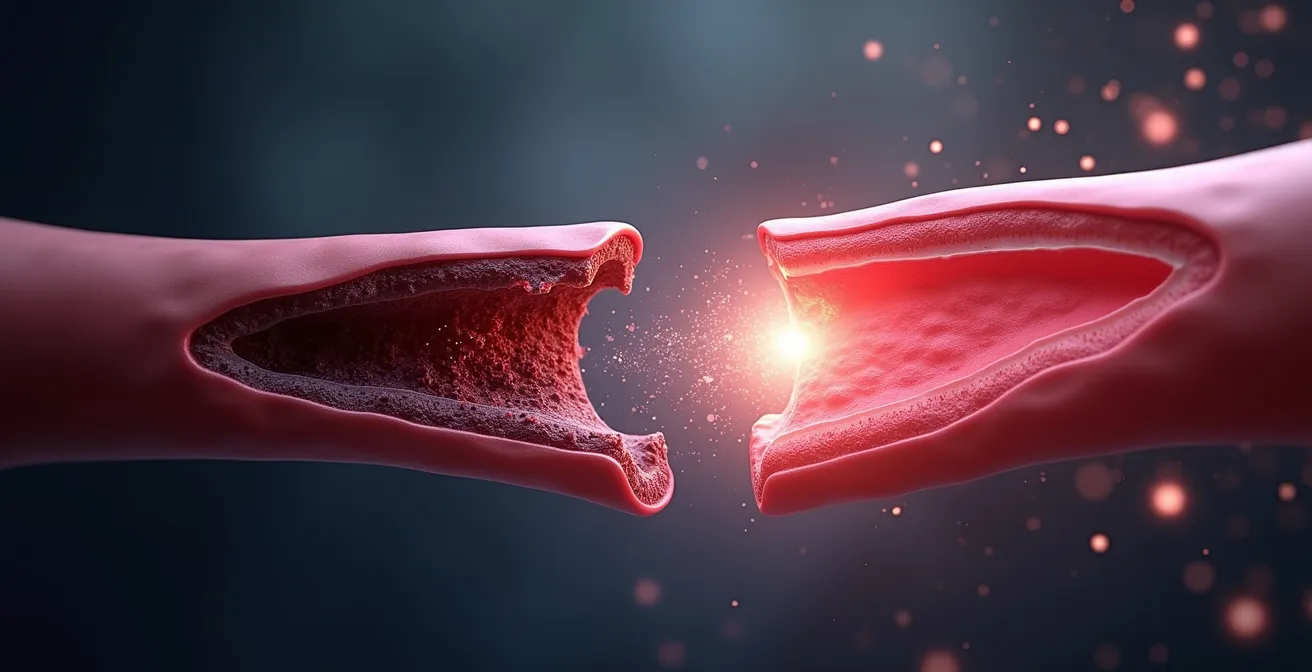
The most immediate and dangerous effect of smoking is not on your lungs, but in your bloodstream. Within minutes of inhaling, hundreds of chemicals trigger a dramatic change in your blood’s consistency. This isn’t a slow, cumulative process; it’s an acute, emergency response. The chemicals cause your platelets—tiny cell fragments responsible for clotting—to become abnormally “sticky.” Instead of flowing smoothly, they begin to clump together, turning your blood from a free-flowing liquid into a more viscous, sludgy substance. Think of it as turning smooth marbles into pieces of Velcro.
This increased stickiness is not a minor side effect. Groundbreaking research from the journal Circulation shows that platelet thrombus formation increases by 200-240% within just five minutes of smoking. This is the very mechanism that forms blood clots. When these clots form in the coronary arteries that feed your heart, they can block blood flow, starving the heart muscle of oxygen and triggering a heart attack. Every cigarette you smoke is essentially a roll of the dice, creating the perfect conditions for a potentially fatal clot to form.
This illustration provides a powerful visual of how platelets activate and begin to aggregate, forming a dangerous mesh. The good news is that this process is reversible. When you stop smoking, your platelets begin to lose their abnormal stickiness within hours. The constant trigger for this hyper-coagulable state is removed, and your blood starts to regain its normal, fluid consistency, dramatically lowering the immediate risk of a clot-related cardiac event.
Statins or Quitting: Which Reduces Cardiovascular Risk More?
Many of my patients who are smokers are also on statins, medications designed to lower cholesterol and reduce cardiovascular risk. They often feel this provides a safety net, but it’s crucial to understand the hierarchy of risk reduction. While statins are a cornerstone of modern cardiology, their impact is significantly overshadowed by the benefits of smoking cessation. Statins work primarily by reducing the amount of cholesterol available to build plaque in your arteries, a process that unfolds over years. Quitting smoking, however, stops the immediate, daily assault on your entire cardiovascular system.
To put this into perspective, a high-potency statin is generally expected to reduce the risk of a major cardiovascular event (like a heart attack or stroke) by about 25-30%. This is a substantial and life-saving benefit. However, the act of quitting smoking is far more powerful. Compelling research presented at the ESC Congress 2024 revealed a 44% reduction in major cardiovascular events among patients who quit smoking after a heart attack. This isn’t a minor difference; quitting is a vastly more effective intervention than starting one of our most effective cardiac medications.
This is because quitting addresses multiple risk factors simultaneously: it lowers blood pressure, reduces blood stickiness, improves oxygen delivery, and calms inflammation in the arteries. A statin primarily addresses one factor: cholesterol. This is why cardiologists are so adamant about cessation.
“I like to tell my patients that it is never too soon or too late to stop smoking, though the sooner a patient stops, the better to lower cardiovascular risk. And it is not enough to reduce smoking. Short, clear messages are needed for smokers at every medical intervention highlighting the need to quit.”
– Dr. Jules Mesnier, ESC Congress 2024
This expert perspective reinforces the clinical data: there is no substitute for quitting. Viewing medication as a license to continue smoking is a dangerous misconception that leaves you exposed to a much higher level of risk.
Tracking Your BP: How Much Does It Drop 2 Weeks After Quitting?
One of the most tangible and motivating signs of recovery is the rapid improvement in your blood pressure (BP). Nicotine is a potent vasoconstrictor, meaning it causes your arteries to tighten and narrow. This forces your heart to work much harder to pump blood through the constricted system, leading to elevated blood pressure. This effect happens with every cigarette, keeping your cardiovascular system in a constant state of stress. When you quit, this pressure begins to release almost immediately.
Within the first 24-48 hours, as nicotine clears from your system, your blood vessels start to relax and widen. Many people see a noticeable drop of 3-5 mmHg in their systolic pressure (the top number) in the first few days. Over the first two weeks, as your body adapts, you can expect this trend to continue. While the most significant, stable reductions are seen over time—one study noted a drop of 6 mmHg systolic after 12 weeks in hypertensive smokers—the initial two-week period is critical for breaking the cycle of nicotine-induced hypertension. This early progress is a powerful motivator.
Tracking this change can be incredibly empowering. It provides concrete, daily evidence that your body is healing. It turns an abstract health goal into a measurable, personal victory. Following a simple plan to monitor your BP can make the benefits of quitting feel real and immediate.
Your 2-Week BP Liberation Tracking Plan
- Establish a Baseline: For the three days before you quit, measure your BP twice daily (morning and evening) after resting for 5 minutes. This is your “smoking BP.”
- Document Day 1: On your first smoke-free day, take your readings at the same times. Note any immediate drop; this is your body’s first thank you.
- Track Withdrawal Spikes (Days 2-7): Continue twice-daily measurements. Don’t be discouraged by small spikes; this can be part of the withdrawal process as your body recalibrates. The overall trend is what matters.
- Observe Stabilization (Week 2): In the second week, your readings should become more consistent at a new, lower level. This is the beginning of your new normal.
- Compare and Celebrate: At the end of week two, calculate your average BP and compare it to your initial baseline. A typical reduction of 5-10 mmHg systolic is a massive win for your heart’s workload.
Why “Cutting Down” to 5 Cigarettes Doesn’t Protect Your Heart?
A common and dangerous myth is that reducing the number of cigarettes to a “light” level—say, under five per day—is a safe long-term strategy. The logic seems sound: less smoke should mean less risk. However, when it comes to cardiovascular disease, the dose-response relationship is not linear. Your heart and blood vessels are incredibly sensitive, and even a small amount of tobacco smoke is enough to keep them in a state of high alert and dysfunction.
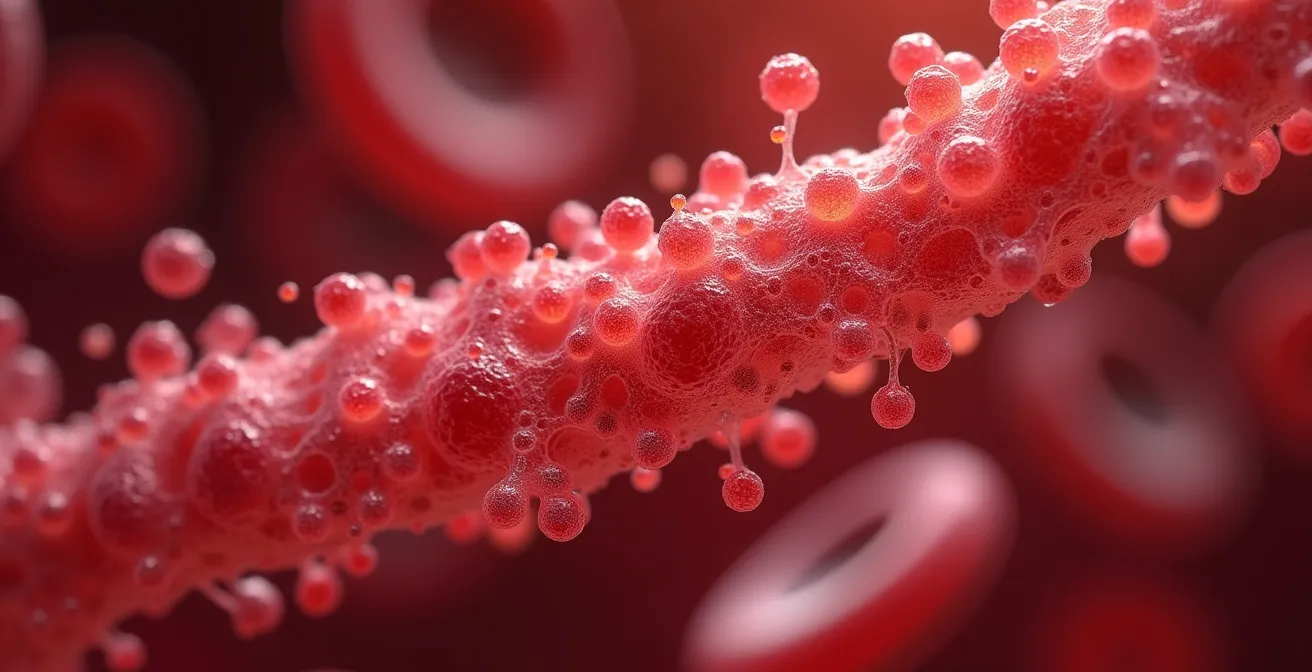
The damage from smoking isn’t just about volume; it’s about the frequency of the inflammatory and clotting triggers. Each cigarette, whether it’s your first or fifteenth of the day, initiates that immediate cascade of platelet activation and arterial constriction. Smoking just one to five cigarettes a day maintains a chronic state of inflammation and endothelial dysfunction (damage to the inner lining of your arteries). You aren’t giving your body the 24-hour smoke-free period it needs to truly begin repairs. It’s like picking a scab every few hours; the wound never gets a chance to heal properly.
The statistics are sobering. Large-scale Australian research involving over 188,000 participants reveals that smoking just 4-6 cigarettes per day carries a 1.92 times higher risk of mortality compared to never-smokers. You are still nearly doubling your risk. Another major study confirmed that smokers who simply reduced their consumption saw no significant change in their risk of major adverse cardiac events compared to those who continued smoking heavily. The only group that saw a dramatic risk reduction was the group that quit completely.
Vitamins and Supplements That Support Artery Health During Recovery
Once you’ve made the pivotal decision to quit, many patients ask if there are supplements that can help accelerate the healing process. It is absolutely critical to understand this: no vitamin or supplement can reverse the damage of smoking or protect you if you continue to smoke. Quitting is the primary therapy. However, certain nutrients can play a supportive role in helping your body repair the oxidative stress and inflammation caused by years of tobacco use.
Smoking depletes the body of crucial antioxidants, particularly Vitamin C. This vitamin is essential for repairing the endothelium, the delicate inner lining of your arteries. It also helps in the production of collagen, a protein vital for maintaining the strength and flexibility of blood vessels. Replenishing Vitamin C through diet (citrus fruits, bell peppers, broccoli) or a moderate supplement can support this repair process.
Another key area is managing inflammation. Omega-3 fatty acids, found in fatty fish like salmon and mackerel or in fish oil supplements, have powerful anti-inflammatory properties. They can help calm the chronic inflammation that smoking has created in your artery walls, making them less prone to plaque rupture. Finally, other antioxidants like Vitamin E and Coenzyme Q10 (CoQ10) can help combat the widespread cellular damage, or “oxidative stress,” left behind by smoking. CoQ10, in particular, is vital for energy production within the heart muscle cells. Always discuss any new supplement regimen with your doctor, as they can interact with medications and may not be appropriate for everyone.
Soft Plaque vs Hard Plaque: The Ticking Time Bomb in Smokers
Not all arterial plaque is created equal. Understanding the difference between soft and hard plaque is critical to grasping the true danger of smoking. Atherosclerosis, the hardening of the arteries, involves the buildup of plaque (a mix of cholesterol, fats, and cellular debris). For a long time, doctors believed the main danger was the size of the plaque—that a large buildup would slowly close off an artery. We now know the real danger lies in the plaque’s stability.
Hard, calcified plaque is like a healed scar. It’s stable, has a thick, fibrous cap, and while it can narrow an artery over time, it’s less likely to cause a sudden, catastrophic event. Your body forms this type of plaque in an attempt to wall off the damage. In contrast, soft, non-calcified plaque is the real ticking time bomb. This type of plaque is inflamed, has a high concentration of fatty lipids, and is covered by a very thin, fragile cap. It’s like a volatile, unstable pimple on the artery wall.
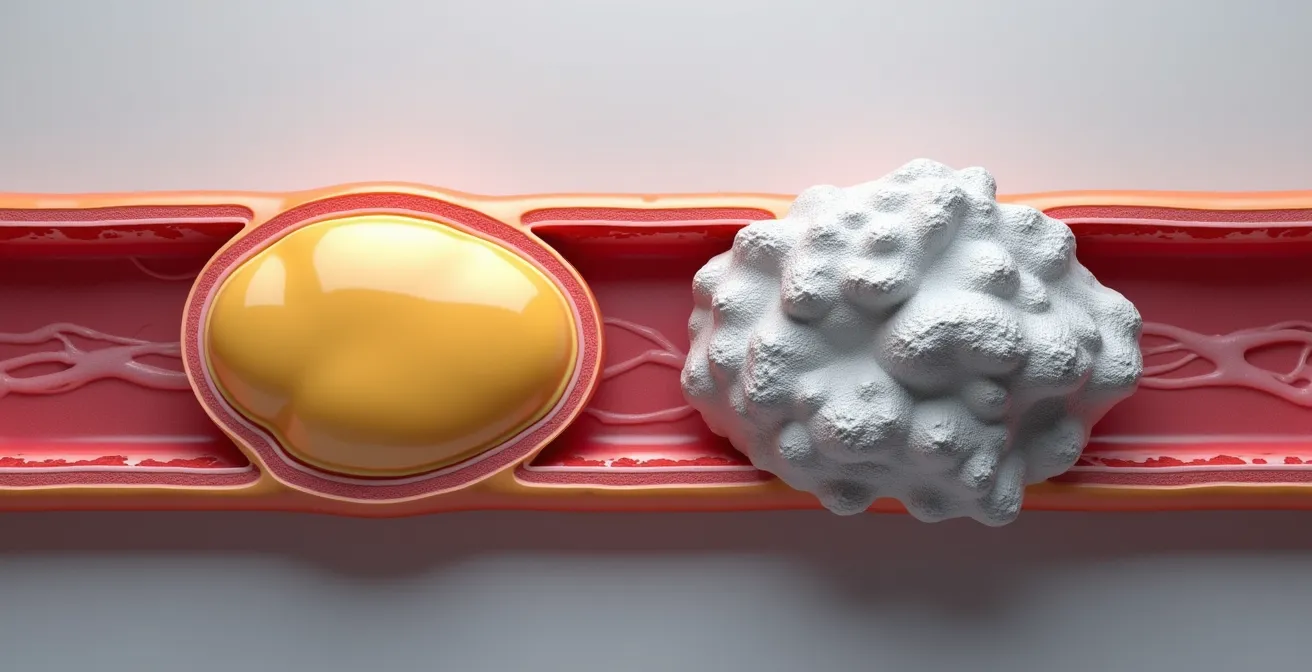
Smoking massively promotes the formation of this dangerous soft plaque. The constant inflammation caused by tobacco smoke makes these plaques more numerous and more likely to rupture. When a soft plaque ruptures, its fatty core is exposed to the bloodstream, triggering the body’s clotting mechanism instantly. A large clot forms on top of the ruptured plaque, completely blocking the artery in minutes. This is the mechanism behind the vast majority of heart attacks in smokers. The good news is that quitting smoking reduces inflammation, allowing the body to begin stabilizing these volatile plaques, slowly converting them from dangerous soft plaques into more stable, scarred-down hard plaques over time.
Why You Feel Tired All Day Despite Sleeping 8 Hours?
One of the most common complaints I hear from my patients who smoke is a pervasive, bone-deep fatigue that a full night’s sleep can’t seem to touch. This isn’t a psychological symptom; it’s a direct result of cellular suffocation caused by carbon monoxide (CO), a major component of cigarette smoke. Your blood contains hemoglobin, a protein in red blood cells whose job is to carry life-giving oxygen to every cell in your body. Carbon monoxide is its arch-nemesis.
The chemical attraction between hemoglobin and carbon monoxide is incredibly strong. In fact, the National Heart, Lung, and Blood Institute explains that CO binds to hemoglobin 200 times more strongly than oxygen. When you smoke, CO floods your bloodstream and hijacks your red blood cells. It latches onto the hemoglobin, refusing to let go. This means there are fewer “seats” available for oxygen to be transported from your lungs to your muscles, brain, and especially your heart muscle. You are creating a state of chronic, low-level oxygen deprivation, or ‘oxygen debt’.
Your body is essentially running on a low battery all day long. Even with 8 hours of sleep, you wake up with CO still circulating in your system, and the first cigarette of the day restarts the cycle. This is why you feel tired, sluggish, and mentally foggy. The recovery from this is remarkably fast. After just 12 hours without a cigarette, the body’s CO levels drop back to normal. Oxygen can once again bind effectively to hemoglobin, and your cells begin receiving the fuel they need. Many people report a surge in energy levels within the first week of quitting, feeling more alert and vibrant than they have in years.
Key Takeaways
- Smoking’s primary cardiac danger is immediate: it makes your blood thicker and stickier within minutes, drastically increasing clot risk.
- Quitting smoking is a more powerful medical intervention for reducing heart attack risk (up to 44% reduction) than starting a statin (25-30% reduction).
- The “cutting down” strategy is a dangerous myth; even 1-5 cigarettes a day maintains chronic inflammation and does not significantly reduce cardiovascular risk.
Silent Ischemia: Why Your Heart Suffers Even Without Chest Pain?
Perhaps the most insidious danger for a long-term smoker is the concept of “silent ischemia.” Ischemia is the medical term for a lack of blood flow and oxygen to a part of the body, and when it happens in the heart, it’s supposed to cause angina—chest pain, pressure, or tightness. This pain is a critical warning signal that your heart muscle is in distress. However, years of smoking can damage the very nerves that are supposed to send these warning signals to your brain. Your heart can be suffering, and you may not feel a thing.
This is why the first symptom of heart disease in a smoker is often not mild chest pain, but a massive, unexpected, and sometimes fatal heart attack. The underlying disease has been progressing silently for years, without the body’s alarm system functioning correctly. You may be experiencing episodes of significant ischemia while walking up a flight of stairs or during a stressful moment, but because the nerve endings are dulled, you simply feel a bit “winded” or tired, dismissing a major red flag.
The statistics on this are chilling. Disturbing American Heart Association research warns that middle-aged male smokers are 1.5 times more likely to have a fatal event as their very first sign of cardiovascular disease. They don’t get the warning shot of angina that a non-smoker might. They are flying blind, unaware of the severe blockages developing in their coronary arteries until it is too late. This is why proactive screening is so essential for smokers over 50. You cannot afford to wait for symptoms that may never arrive.
The evidence is clear: the most powerful prescription for your heart health is the decision to quit. Your journey to a stronger heart doesn’t start in a year or a month; it begins the moment you extinguish your last cigarette. The next logical step is to create a tangible quit plan and discuss it with your healthcare provider to get the support you need.
Frequently Asked Questions About Smoking and Heart Health After 50
What screening tests should smokers over 50 request?
Beyond standard cholesterol and blood pressure checks, it’s wise to discuss more advanced screening with your doctor. Tests like a coronary calcium score (a CT scan that measures hard plaque), a stress test (to see how your heart responds to exertion), or even a CT angiogram can help detect silent ischemia and significant blockages before they cause a heart attack.
How quickly does quitting restore warning sensitivity?
This is a difficult area to predict. Some nerve function may partially recover over months or years, but significant nerve damage can be permanent. The primary focus should always be on proactive screening and aggressive risk factor reduction (quitting, controlling BP, and cholesterol) rather than waiting for warning symptoms like chest pain to return. Assume the alarm system is faulty and use medical tools to check for fire instead.